|
|
|
|
|
FMD | 精彩荐读:中国成年人睡眠模式及其他行为的等时间替代与慢性肾脏病(CKD)患病率的关联 |
|
|
论文标题:Associations of sleeping patterns and isotemporal substitution of other behavior with the prevalence of CKD in Chinese adults
期刊: Frontiers of Medicine
作者:Yi Ding, Xiaoli Xu, Zhuojun Xin, Qiuyu Cao, Jiaojiao Huang,Xianglin Wu, Yanan Huo , Qin Wan,Yingfen Qin, Ruying Hu,Lixin Shi,Qing Su, Xuefeng Yu,Li Yan, Guijun Qin , Xulei Tang, Gang Chen, Min Xu,Tiange Wang ,Zhiyun Zhao, Zhengnan Gao, Guixia Wang, Feixia Shen, Zuojie Luo, Li Chen,Qiang Li, Zhen Ye,Yinfei Zhang, Chao Liu , Youmin Wang, Tao Yang, Huacong Deng,Lulu Chen, Tianshu Zeng, Jiajun Zhao, Yiming Mu, Shengli Wu, Yuhong Chen,Jieli Lu, Weiqing Wang, Guang Ning ,Yu Xu, Yufang Bi , Mian Li
发表时间: 15 Apr 2024
DOI:10.1007/s11684-023-1019-5
微信链接:点击此处阅读微信文章
导 读
上海交通大学医学院附属瑞金医院李勉、毕宇芳、Yu Xu等在Frontiers of Medicine发表研究论文《中国成年人睡眠模式及其他行为的等时间替代与慢性肾脏病(CKD)患病率的关联》(Associations of sleeping patterns and isotemporal substitution of other behavior with the prevalence of CKD in Chinese adults)。本研究通过探讨我国成年人睡眠模式与慢性肾病患病率的关联,发现睡眠时长与慢性肾病呈U型关系,长睡眠者将1小时睡眠替换为步行、中高强度体力活动或久坐可降低患病率,糖尿病患者等亚群获益显著。
慢性肾病(CKD)作为全球重大的公共卫生问题,其高死亡率和进展性特征给亚洲地区带来了沉重的疾病负担。肾脏功能的保护可通过生活方式干预实现,而睡眠作为占据人一生近三分之一时间的行为因素,近年来被证实与公共健康密切相关。已有研究表明,睡眠时长与慢性肾病风险之间存在U型关系,即睡眠不足(少于6小时)或睡眠过长(超过8小时)均可能增加患病风险。然而,现有研究多聚焦于睡眠时长本身与慢性肾病的关联,较少探讨通过调整整体日常行为组成来优化睡眠模式以改善肾脏健康的可能性。等时替代模型(ISMs)为这类研究提供了方法学支持,该模型能够分析不同活动模式的时间分配与健康结局的关联,但此前尚未有研究系统应用该模型探讨过多睡眠与其他行为的替代效应对慢性肾病的影响。
上海交通大学医学院附属瑞金医院李勉、毕宇芳、Yu Xu等通过收集我国糖尿病患者癌症风险评估纵向研究中的104538名成年参与者的日常睡眠、久坐、步行及中高强度体力活动时间,并结合临床检测指标分析了这些行为与慢性肾病患病率的关联。研究采用横断面设计,参与者的睡眠时长通过问卷收集近7天的平均夜间睡眠时间,久坐时间通过工作日和周末的每日久坐时长计算,体力活动则采用国际体力活动问卷短卷评估,分为步行和中高强度体力活动,其中中高强度体力活动进一步区分为职业体力活动(OPA)和休闲时间体力活动(LTPA)。慢性肾病的诊断依据改善全球肾脏病预后组织(KDIGO)2012年指南,定义为估算肾小球滤过率<60 mL/min/1.73m2或尿白蛋白/肌酐比值≥30 mg/g。统计分析中,研究首先通过限制性立方样条模型验证了睡眠时长与慢性肾病患病率的非线性关系,随后采用等时替代模型,在控制总时间和其他行为的前提下,分析将1小时睡眠分别替换为久坐、步行或中高强度体力活动时的患病风险变化,并通过分层分析探讨不同工作状态(在职/失业)、睡眠时长(<8小时/≥8小时)、就寝时间(≤23:00/>23:00)及血糖状态(正常血糖、糖尿病前期、糖尿病)对结果的影响。研究结果显示,参与者中5.0%睡眠不足6小时,29.0%睡眠6-8小时,66.0%睡眠≥8小时,长睡眠者的慢性肾病患病率显著高于理想睡眠组。限制性立方样条分析证实了睡眠时长与慢性肾病患病率的U型关系,其中长睡眠与尿白蛋白/肌酐比值异常的关联更为显著,而与估算肾小球滤过率下降的关联较弱(图1)。等时替代模型分析发现,将1小时长睡眠替换为久坐、步行或中高强度体力活动,均与慢性肾病患病率降低相关,对应的比值比(OR)分别为0.98、0.95和0.96。在体力活动类型中,休闲时间体力活动的替代效果优于职业体力活动,例如在职人群中,将1小时睡眠替换为休闲时间体力活动可使慢性肾病患病率降低12%,而替换为职业体力活动仅降低5%-8%。分层分析显示,上述获益主要集中于长睡眠者(≥8小时),且早睡者(就寝时间≤23:00)的获益更为显著(图2);在血糖状态分层中,糖尿病患者将长睡眠替换为步行或中高强度体力活动时,慢性肾病患病率的降低幅度大于糖尿病前期人群(图3)。此外,研究还发现,将久坐时间替换为步行或中高强度体力活动也与慢性肾病风险降低相关,且中高强度体力活动对降低重度慢性肾病的效果更为突出。
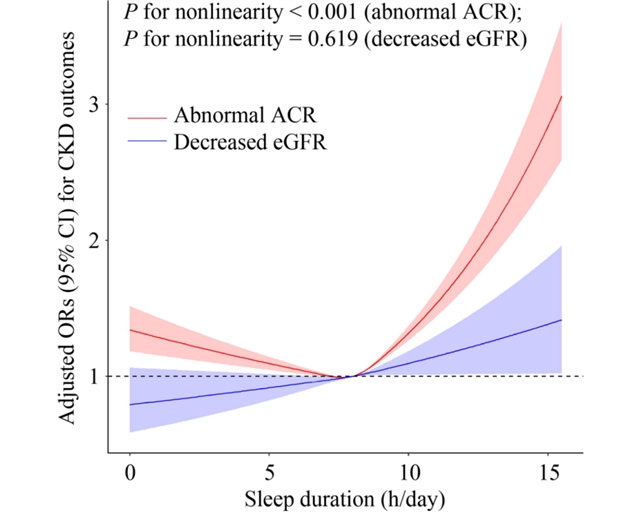
图1 睡眠时间与异常尿白蛋白/肌酐比值及估算肾小球滤过率降低的比值比的关联
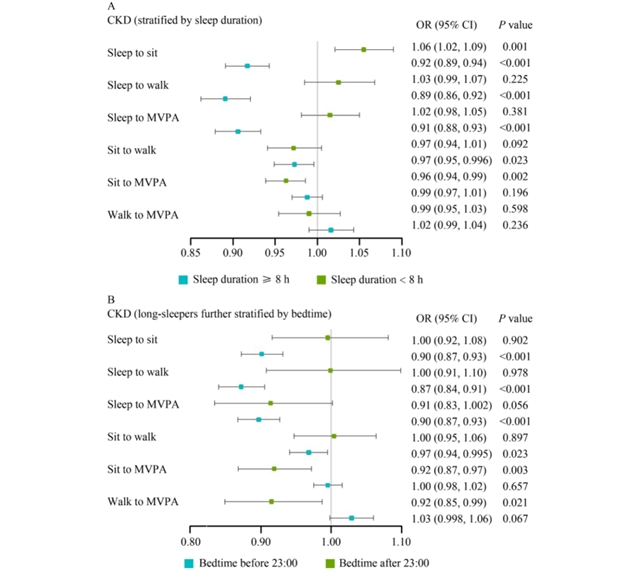
图2 按睡眠时间分层并进一步按就寝时间分层时,重新分配1小时睡眠、久坐、步行及中高强度体力活动与慢性肾脏病结局的关联
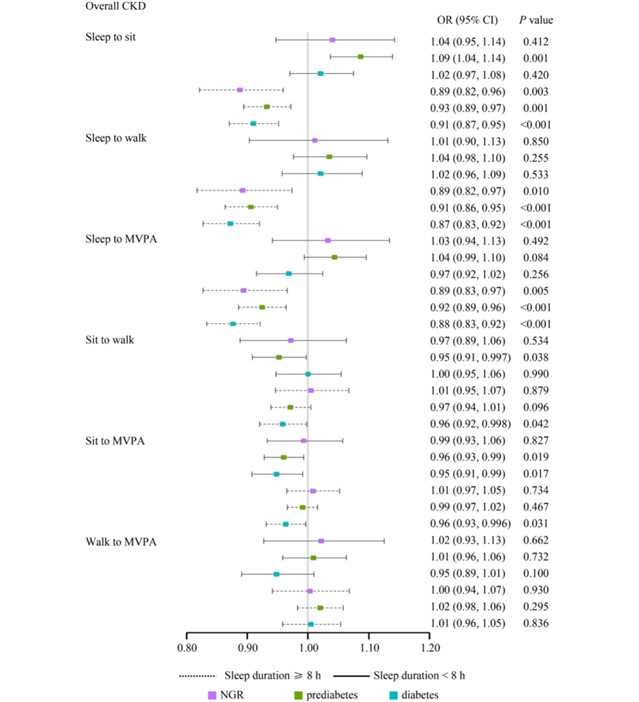
图3 在不同血糖状态(包括正常血糖调节、糖尿病前期及糖尿病)参与者中,按睡眠时间分层时,重新分配1小时睡眠、久坐、步行及中高强度体力活动与总体慢性肾脏病患病率的关联
本研究应用等时替代模型探讨了过多睡眠与其他日常行为的时间分配对慢性肾病的影响,为慢性肾病的行为干预提供了新的视角。研究证实,即使将过多睡眠替换为通常被认为是高风险行为的久坐,也能降低慢性肾病患病率,这可能是因为与久坐相比,过长睡眠是一种更“不活跃”的行为模式,可能通过加剧肌肉萎缩、炎症反应及肾脏昼夜节律紊乱等机制增加肾脏负担。同时,研究发现休闲时间体力活动的保护效应优于职业体力活动,支持了“体力活动悖论”在慢性肾病领域的适用性,即职业体力活动可能因强度低、持续时间长或伴随不良工作姿势而无法带来健康获益,甚至可能升高血压和炎症水平。这些发现提示,针对长睡眠者,尤其是早睡的糖尿病患者,临床实践中可优先推荐增加休闲时间的步行或中高强度体力活动,以替代过多的睡眠。
原文信息
标题
Associations of sleeping patterns and isotemporal substitution of other behavior with the prevalence of CKD in Chinese adults
作者
Yi Ding1,2, Xiaoli Xu1,2, Zhuojun Xin1,2, Qiuyu Cao1,2, Jiaojiao Huang1,2, Xianglin Wu1,2, Yanan Huo3, Qin Wan4, Yingfen Qin5, Ruying Hu6, Lixin Shi7, Qing Su8, Xuefeng Yu9, Li Yan10, Guijun Qin11, Xulei Tang12, Gang Chen13, Min Xu1,2, Tiange Wang1,2, Zhiyun Zhao1,2, Zhengnan Gao14, Guixia Wang15, Feixia Shen16, Zuojie Luo5, Li Chen17, Qiang Li18, Zhen Ye6, Yinfei Zhang19, Chao Liu20, Youmin Wang21, Tao Yang22, Huacong Deng23, Lulu Chen24, Tianshu Zeng24, Jiajun Zhao25, Yiming Mu26, Shengli Wu27, Yuhong Chen1,2, Jieli Lu1,2, Weiqing Wang1,2, Guang Ning1,2, Yu Xu1,2, Yufang Bi1,2, Mian Li1,2
机构
1. Department of Endocrine and Metabolic Diseases, Shanghai Institute of Endocrine and Metabolic Diseases, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200025, China
2. Shanghai National Clinical Research Center for Metabolic Diseases, Key Laboratory for Endocrine and Metabolic Diseases of the National Health Commission of China, Shanghai Key Laboratory for Endocrine Tumor, State Key Laboratory of Medical Genomics, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200025, China
3. Jiangxi Provincial People’s Hospital, Affiliated to Nanchang University, Nanchang 330000, China
4. Department of Endocrinology, The Affiliated Hospital of Southwest Medical University, Luzhou 646000, China
5. Department of Endocrinology, The First Affiliated Hospital of Guangxi Medical University, Nanning 530000, China
6. Zhejiang Provincial Center for Disease Control and Prevention, Hangzhou 310000, China
7. Department of Endocrinology, Affiliated Hospital of Guiyang Medical University, Guiyang 550000, China
8. Xinhua Hospital, Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai 200000, China
9. Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430000, China
10. Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou 510000, China
11. Department of Endocrinology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, China
12. Department of Endocrinology, The First Hospital of Lanzhou University, Lanzhou 730000, China
13. Fujian Provincial Hospital, Fujian Medical University, Fuzhou 350000, China
14. Dalian Municipal Central Hospital, Affiliated of Dalian Medical University, Dalian 116000, China
15. Department of Endocrinology, The First Hospital of Jilin University, Changchun 130000, China
16. Department of Endocrinology, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou 325000, China
17. Qilu Hospital of Shandong University, Jinan 250000, China
18. Department of Endocrinology, The Second Affiliated Hospital of Harbin Medical University, Harbin 150000, China
19. Department of Endocrinology, Central Hospital of Shanghai Jiading District, Shanghai 200000, China
20. Department of Endocrinology, Jiangsu Province Hospital on Integration of Chinese and Western Medicine, Nanjing 210000, China
21. Department of Endocrinology, The First Affiliated Hospital of Anhui Medical University, Hefei 230000, China
22. Department of Endocrinology, The First Affiliated Hospital of Nanjing Medical University, Nanjing 210000, China
23. Department of Endocrinology, The First Affiliated Hospital of Chongqing Medical University, Chongqing 410000, China
24. Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430000, China
25. Shandong Provincial Hospital, Affiliated to Shandong University, Jinan 250000, China
26. Department of Endocrinology, Chinese People’s Liberation Army General Hospital, Beijing 100000, China
27. Department of Endocrinology, Karamay Municipal People’s Hospital, Karamay 834000, China
通讯作者
Yu Xu, Yufang Bi, Mian Li
引用这篇文章
Yi Ding, Xiaoli Xu, Zhuojun Xin, Qiuyu Cao, Jiaojiao Huang, Xianglin Wu, Yanan Huo, Qin Wan, Yingfen Qin, Ruying Hu, Lixin Shi, Qing Su, Xuefeng Yu, Li Yan, Guijun Qin, Xulei Tang, Gang Chen, Min Xu, Tiange Wang, Zhiyun Zhao, Zhengnan Gao, Guixia Wang, Feixia Shen, Zuojie Luo, Li Chen, Qiang Li, Zhen Ye, Yinfei Zhang, Chao Liu, Youmin Wang, Tao Yang, Huacong Deng, Lulu Chen, Tianshu Zeng, Jiajun Zhao, Yiming Mu, Shengli Wu, Yuhong Chen, Jieli Lu, Weiqing Wang, Guang Ning, Yu Xu, Yufang Bi, Mian Li Associations of sleeping patterns and isotemporal substitution of other behavior with the prevalence of CKD in Chinese adults. Frontiers of Medicine, 2024, 18(2): 303-314
https://doi.org/10.1007/s11684-023-1019-5
https://journal.hep.com.cn/fmd/EN/10.1007/s11684-023-1019-5
https://link.springer.com/article/10.1007/s11684-023-1019-5
《前沿》系列英文学术期刊
由教育部主管、高等教育出版社主办的《前沿》(Frontiers)系列英文学术期刊,于2006年正式创刊,以网络版和印刷版向全球发行。系列期刊包括基础科学、生命科学、工程技术和人文社会科学四个主题,是我国覆盖学科最广泛的英文学术期刊群,其中12种被SCI收录,其他也被A&HCI、Ei、MEDLINE或相应学科国际权威检索系统收录,具有一定的国际学术影响力。系列期刊采用在线优先出版方式,保证文章以最快速度发表。
中国学术前沿期刊网
http://journal.hep.com.cn

特别声明:本文转载仅仅是出于传播信息的需要,并不意味着代表本网站观点或证实其内容的真实性;如其他媒体、网站或个人从本网站转载使用,须保留本网站注明的“来源”,并自负版权等法律责任;作者如果不希望被转载或者联系转载稿费等事宜,请与我们接洽。