德克萨斯大学Moran Amit研究组宣布他们发现了癌症诱导的神经损伤促进抗PD-1治疗的耐药性。这一研究成果发表在2025年8月20日出版的国际学术期刊《自然》上。
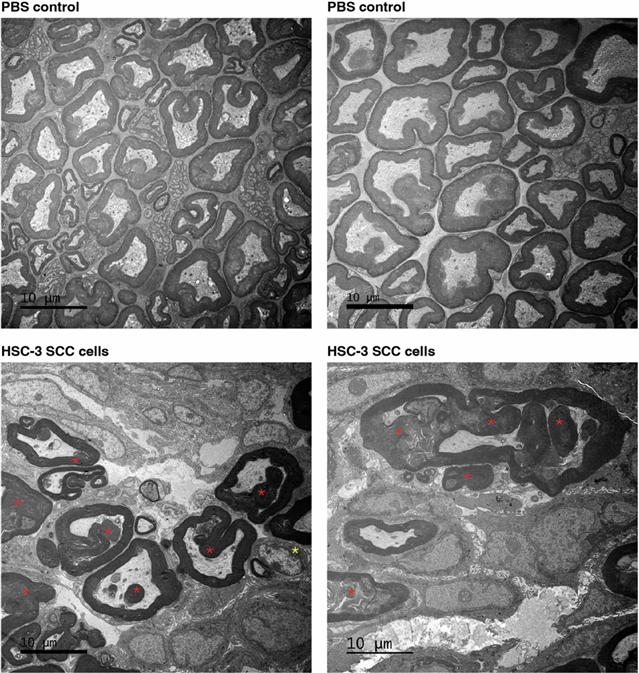
在这里,该课题组人员提供了PNI和癌症诱导的神经损伤(CINI)在抗PD-1治疗耐药中的作用的临床和机制见解。他们的研究表明,在皮肤鳞状细胞癌、黑色素瘤和胃癌患者中,肿瘤相关神经的PNI和CINI与抗PD-1治疗反应较差有关。电子显微镜和电导分析显示,癌细胞降解神经纤维髓鞘片。损伤神经元通过自主启动IL-6和I型干扰素介导的炎症反应来促进神经愈合和再生。随着肿瘤的生长,CINI负担增加,其相关炎症变为慢性,并使肿瘤微环境中的一般免疫基调进入抑制和衰竭状态。可以通过靶向CINI信号传导过程中的多个步骤来逆转CINI驱动的抗PD-1抗性:使肿瘤失神经,有条件地敲除介导神经元内损伤信号的转录因子(Atf3),敲除干扰素α受体信号(Ifnar1/)或联合抗PD-1和抗IL-6受体阻断。他们的发现证明了CINI的直接免疫调节作用及其治疗潜力。
据了解,围神经侵犯(PNI)是多种1型癌症预后不良的一个公认因素,但其机制尚不清楚。
附:英文原文
Title: Cancer-induced nerve injury promotes resistance to anti-PD-1 therapy
Author: Baruch, Erez N., Gleber-Netto, Frederico O., Nagarajan, Priyadharsini, Rao, Xiayu, Akhter, Shamima, Eichwald, Tuany, Xie, Tongxin, Balood, Mohammad, Adewale, Adebayo, Naara, Shorook, Sathishkumar, Hinduja N., Islam, Shajedul, McCarthy, William, Mattson, Brandi J., Ferrarotto, Renata, Wong, Michael K., Davies, Michael A., Jindal, Sonali, Basu, Sreyashi, Roversi, Karine, Nikpoor, Amin Reza, Ahmadi, Maryam, Ahmadi, Ali, Harwood, Catherine, Leigh, Irene, Gong, Dennis, Talln de Lara, Paulino, Tao, Derrick L., Davidson, Tara M., Ajami, Nadim J., Futreal, Andrew, Rai, Kunal, Kochat, Veena, Castillo, Micah, Gunaratne, Preethi, Goepfert, Ryan P., Hernandez, Sharia D., Khushalani, Nikhil I., Wang, Jing, Watowich, Stephanie S., Calin, George A., Migden, Michael R., Yuan, Mona, Liu, Naijiang, Ye, Yi, Hwang, William L., Vermeer, Paola D., DSilva, Nisha J., Bunimovich, Yuri L., Yaniv, Dan, Burks, Jared K., Gomez, Javier, Dougherty, Patrick M., Tsai, Kenneth Y., Allison, James P., Sharma, Padmanee, Wargo, Jennifer A., Myers, Jeffrey N., Talbot, Sebastien, Gross, Neil D., Amit, Moran
Issue&Volume: 2025-08-20
Abstract: Perineural invasion (PNI) is a well-established factor of poor prognosis in multiple cancer types1, yet its mechanism remains unclear. Here we provide clinical and mechanistic insights into the role of PNI and cancer-induced nerve injury (CINI) in resistance to anti-PD-1 therapy. Our study demonstrates that PNI and CINI of tumour-associated nerves are associated with poor response to anti-PD-1 therapy among patients with cutaneous squamous cell carcinoma, melanoma and gastric cancer. Electron microscopy and electrical conduction analyses reveal that cancer cells degrade the nerve fibre myelin sheets. The injured neurons respond by autonomously initiating IL-6- and type I interferon-mediated inflammation to promote nerve healing and regeneration. As the tumour grows, the CINI burden increases, and its associated inflammation becomes chronic and skews the general immune tone within the tumour microenvironment into a suppressive and exhaustive state. The CINI-driven anti-PD-1 resistance can be reversed by targeting multiple steps in the CINI signalling process: denervating the tumour, conditional knockout of the transcription factor mediating the injury signal within neurons (Atf3), knockout of interferon-α receptor signalling (Ifnar1/) or by combining anti-PD-1 and anti-IL-6-receptor blockade. Our findings demonstrate the direct immunoregulatory roles of CINI and its therapeutic potential.
DOI: 10.1038/s41586-025-09370-8
Source: https://www.nature.com/articles/s41586-025-09370-8
Nature:《自然》,创刊于1869年。隶属于施普林格·自然出版集团,最新IF:69.504
官方网址:http://www.nature.com/
投稿链接:http://www.nature.com/authors/submit_manuscript.html
