|
|
|
|
|
哪些药物可以降低急诊住院率 | BMC Medicine |
|
|
论文标题:Medications that reduce emergency hospital admissions: an overview of systematic reviews and prioritisation of treatments
期刊:BMC Medicine
作者:Niklas Bobrovitz et al
发表时间: 2018/7/26
数字识别码:10.1186/s12916-018-1104-9
原文链接:https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-018-1104-9?utm_source=WeChat&utm_medium=Social_media_organic&utm_content=DaiDen-BMC-BMC_Medicine-Immunology-China&utm_campaign=BMCF_USG_BSCN_DD_BM_BLOG
微信搜索BMC期刊,获取最新期刊资讯、论文解析、投稿建议等实用信息。
有效减少患者急诊入院次数的药物在患者治疗中极具价值。BMC Medicine上发表的一项新研究共参考了140篇系统评价,找到了11种具有这类效果的药物,虽然其中大部分药物已经常规应用于临床实践,但其实际临床使用情况差异较大,这意味着这一领域仍有进一步改进的空间。让我们来听听这篇文章作者之一Niklas Bobrovitz的详细介绍。

急诊入院人数的不断上升使得政策制定人员、临床医生和患者越来越担心随之产生的一系列影响,例如选择性治疗的取消、被延长的入院等待时间以及住院感染风险和医疗费用等。但想要找到有效的应对策略并不容易,一些旨在降低住院率的干预措施并未发挥实际作用,却消耗了本已非常稀少的医疗资源。
其中一种前景颇佳但受关注程度却很少的干预措施就是药物治疗。能够有效减少患者急诊入院次数的药物在患者总体治疗过程中极具价值。药物治疗可以预防疾病,并缓解某些需要紧急治疗的疾病症状以及其恶化程度,从而降低住院率。
因此,我们发表在BMC Medicine的研究旨在通过查阅系统评价,发现并优化那些可能降低急诊入院率的药物干预治疗。
我们做了什么?
我们搜索了关于以住院为结局的成人随机对照试验系统评价。数据质量以GRADE标准评估。我们将文献中找到的具有中/高证据质量的有效药物与英国、美国和欧洲临床指南交叉比对以进一步明确使用哪些药物的利害平衡在可接受范围内。
我们发现了什么?
我们共找到140项系统评价,包括1,968项随机对照试验和925,364名患者。经过分析确定了11种能降低急诊住院率的药物,这些发现都有中/高质量等级的证据支持,也得到了临床指南的认可。
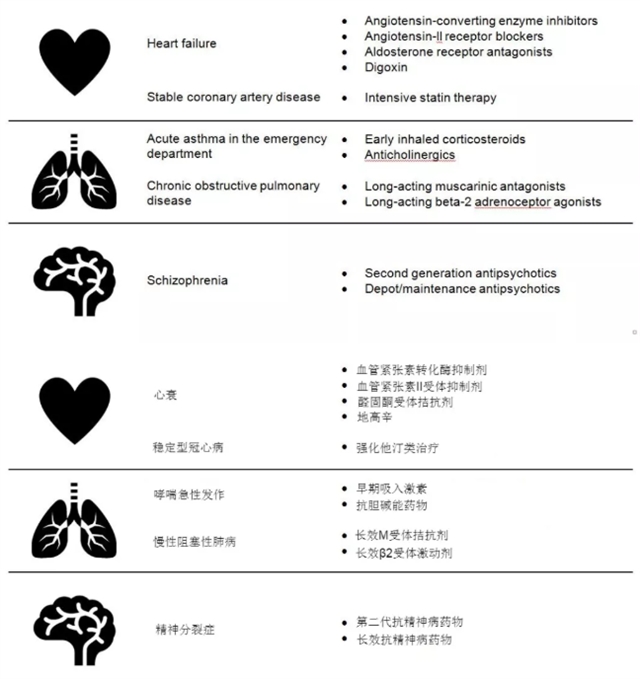
基于研究证据且受指南支持的可降低急诊入院率的药物中英对照表
这些发现意味着什么?
我们所确定的11种药物在临床上适用于心衰、冠心病、哮喘、慢性阻塞性肺病和精神病患者,并会显著降低这些患者的急诊入院率。
在部分国家或地区的医疗体系中,这些药物已经常规用于临床实践。但有证据表明这些药物在英国、美国和欧洲的使用存在显著差异,包括使用不充分、剂量不足等情况。因此,政策制定者和临床医生应考虑将监测和改善这些药物的使用作为减轻急诊压力的干预策略。
我们可以利用现有的质量评估和改进机制。例如,英国质量-成果框架(Quality and Outcomes Framework )是一项按业绩付酬的激励计划,该计划的推行增加了药物使用并提高了处方效率。我们所挑选的药物也应当纳入这类质量保证和激励系统中。
我们的结果也为医生-患者共同决策提供了信息。在与符合条件的患者沟通治疗方案时,临床医生应该告知患者这些药物可以降低住院风险。考虑到大多数患者都不愿意住院,我们希望这些研究结果能为他们的决策提供信息。
摘要:
Background
Rates of emergency hospitalisations are increasing in many countries, leading to disruption in the quality of care and increases in cost. Therefore, identifying strategies to reduce emergency admission rates is a key priority. There have been large-scale evidence reviews to address this issue; however, there have been no reviews of medication therapies, which have the potential to reduce the use of emergency health-care services. The objectives of this study were to review systematically the evidence to identify medications that affect emergency hospital admissions and prioritise therapies for quality measurement and improvement.
Methods
This was a systematic review of systematic reviews. We searched MEDLINE, PubMed, the Cochrane Database of Systematic Reviews & Database of Abstracts of Reviews of Effects, Google Scholar and the websites of ten major funding agencies and health charities, using broad search criteria. We included systematic reviews of randomised controlled trials that examined the effect of any medication on emergency hospital admissions among adults. We assessed the quality of reviews using AMSTAR. To prioritise therapies, we assessed the quality of trial evidence underpinning meta-analysed effect estimates and cross-referenced the evidence with clinical guidelines.
Results
We identified 140 systematic reviews, which included 1968 unique randomised controlled trials and 925,364 patients. Reviews contained 100 medications tested in 47 populations. We identified high-to moderate-quality evidence for 28 medications that reduced admissions. Of these medications, 11 were supported by clinical guidelines in the United States, the United Kingdom and Europe. These 11 therapies were for patients with heart failure (angiotensin-converting-enzyme inhibitors, angiotensin II receptor blockers, aldosterone receptor antagonists and digoxin), stable coronary artery disease (intensive statin therapy), asthma exacerbations (early inhaled corticosteroids in the emergency department and anticholinergics), chronic obstructive pulmonary disease (long-acting muscarinic antagonists and long-acting beta-2 adrenoceptor agonists) and schizophrenia (second-generation antipsychotics and depot/maintenance antipsychotics).
Conclusions
We identified 11 medications supported by strong evidence and clinical guidelines that could be considered in quality monitoring and improvement strategies to help reduce emergency hospital admission rates. The findings are relevant to health systems with a large burden of chronic disease and those managing increasing pressures on acute health-care services.
阅读论文原文,请访问
https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-018-1123-6?utm_source=Other_website&utm_medium=Website_links&utm_content=DaiDen-BMC-BMC_Medicine-Public_Health-China&utm_campaign=BMCF_USG_BSCN_DD_BMCMedicine
(来源:科学网)
特别声明:本文转载仅仅是出于传播信息的需要,并不意味着代表本网站观点或证实其内容的真实性;如其他媒体、网站或个人从本网站转载使用,须保留本网站注明的“来源”,并自负版权等法律责任;作者如果不希望被转载或者联系转载稿费等事宜,请与我们接洽。